The only nice thing about being a cancer patient is that you get lots of sympathy. Over the next few weeks, as my treatment progressed, both old and new friends came to visit, I was sent cards, and I received some lovely flowers.

My regime was written out on a photocopied information sheet. 11 weeks of chemotherapy tablets, plus additional chemotherapy infusions given by drip intravenously (IV) every 3 weeks, and in the last 5 weeks I would be having radiotherapy too.
One Wednesday 4th October, 2023, I went to the Christie Hospital for my first round of IV infusions. I walked to the hospital – a distance of around 3 miles. When I arrived, I was allocated to an area and a team. As I walked through the chemo unit, I discovered it was huge, and we sat in reclining chairs, not beds. The unit was cleverly arranged with curving corridors, so that you could only see a handful of people in chairs on either side and opposite.
I was there for 9 long hours. The actual chemotherapy didn’t take 9 hours. I needed to watch an introductory video first, then I had a steroid infusion, followed by an anti-sickness infusion, next a massive bag of special fluid to protect my kidneys, then the actual chemotherapy (which took 2 hours), and another bag of special fluid for my kidneys. Inbetween each of these, I had a small bag of normal saline to flush the system through.
Of course, with all this fluid going in, I had to keep going to the toilet. This involved pulling / pushing my infusion pump with me to the nearest loo, and then navigating the act of using the toilet with only one hand. A tricky business.
Amazingly, after all this, I felt quite well for a couple of days. My brother, Paul, came to stay to look after me but I felt a fraud. This chemo business was a piece of cake!
I had started some twice-daily chemo tablets too, and temporarily I was on steroids and heavy-duty anti-sickness medication. It was a complicated regime, and I used a notebook to tick off my medication and set my iPhone with bleep reminders. As I have previously noted, it really is a full time job being a cancer patient!
After a few days, the steroid and sickness medications were tailed off – and my condition plummeted. By Monday I could barely get out of bed. Paul had to leave, and my youngest daughter came to stay for a few nights. “Oh, mum, you can’t last 11 weeks like this,” she said. I agreed.
But, the next day I felt a bit better and, by the following Tuesday, I was feeling almost back to normal. Well enough, in fact, to go out for walks with my eldest daughter and granddaughter in one of our local parks. We were having a lovely autumn, and I enjoyed the sunshine and walking among the interesting trees.

I also had to go in for a radiotherapy planning session, which involved lying in a very unfomfortable postion (arms above head) for 20 minutes while the CT scanner and the computer drew up a complex image of my tumour so that the radiotherapy could be targeted. I was also given three tiny tattoos. (My first – and only – tattoos!)
After a chat with the oncologist, she changed my antisickness infusion to a more effective drug. And I had my second IV infusion on Wednesday, 25th October. This time, I was only in the unit for 7 hours. I slept most of the time, only woken by the bleep the machine made when the bag needed changing to a different drug. Or when I had to go to the loo.
When I left the unit at the end of the day, I realised that all the other patients around me had changed, or gone home. I had been one of the first patients to arrive, and was one of the last to leave. It was a long day.
My brother Paul came again, and my daughter, Annie, took over when he left. I still felt sick and awful the following Sunday and Monday, but not as bad as the first time. The trouble is, I didn’t bounce back as I had after the first treatment. Very disappointing to find myself so tired and lethargic.
That wasn’t the only problem. I had been told that my swallowing might improve dramatically with the chemotherapy. Unfortunately, my swallowing, in fact, got a bit worse, with loud gurgling whenever I ate. On Tuesday, 2nd November, I had a very distressing episode when a mouthful of salmon and mashed potato got stuck. It cleared eventually.
“Have to face the fact that probably the chemo isn’t working,” I wrote in my diary.
This was a dismal time. I don’t like November anyway, with the darkening days. The sunlight of October had given way to drizzle and rain. “My JIG tube had been given me trouble with soreness and leaking around the three “buttons” that held it in place. “Feel my life is slipping away in a haze of fatigue and nausea,” I wrote. “Too tired and sicky to do anything constructive.”
One bright point was when my lovely son-in-law drove me back to Anglesey. We only stayed one night, arriving in the evening and leaving the following evening. But I got to spend a day on the beach. Windy and wild, but lovely to be here.

Back in Manchester, I could still make it out to the shops, and so I stocked up on instant porridge and cartons of eggs, filled the freezer with ice cream, and the cupboard with bars of chocolate. I swear it was chocolate that kept me going during these dark days. In fact, I managed NOT to lose any weight – which I put down to my regular intake of one large Cadbury’s Dairy Milk with Hazlenut bar a day!
But I was too tired to visit my favourite tree. Here is a photo I took earlier in October, sad that this was probably the last time I would visit it. (It’s a young white oak, in case you are wondering.)

On Monday the 13th November, I started my radiotherapy. I had been dreading it, but there seemed nothing to it. The whole session lasted 10 minutes or so. There was no pain. And, when I looked around everyone in the waiting room looked so ill. People were in wheelchairs. Thank goodness I’m not as bad as THAT I thought to myself.
The next day, I combined my radiotherapy visit with a visit to the blood test room, for a routine blood test in preparation for my third round of IV chemotherapy, which was due the next day. That afternoon, the radiotherapy people phoned me. My neutrophils were low (one of the types of white blood cells that help you fight infection). I should defer my chemo infusion for a week, and stop the chemotherapy tablets I was taking regularly.
Of course, I had mixed feelings about this. I was glad to defer the awful IV chemo for a week, but knew I was only prolonging the length of the treatment time.
Going for radiotherapy every day kept me busy. I took an Uber cab there and back again – because I really didn’t feel up to driving. When I started going, the cab drivers often asked if I worked at the Christie – because, I guess, I looked quite well. In fact, everyone who visited said how well I looked!
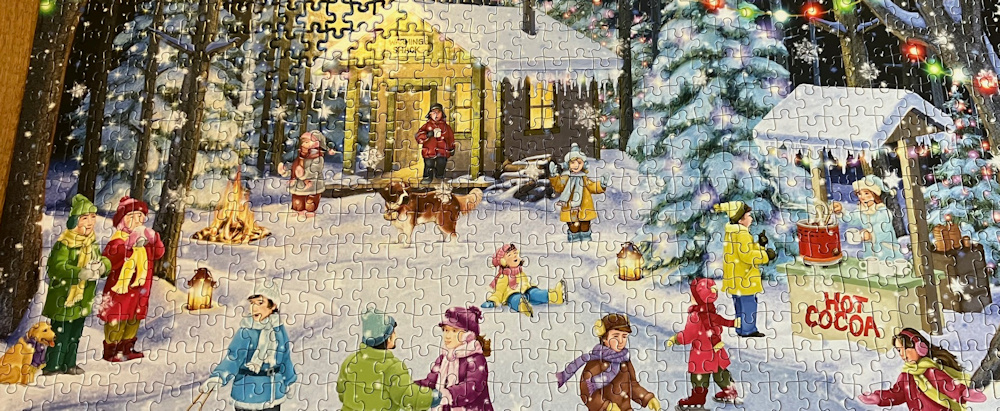
But, I didn’t feel well. I couldn’t concentrate on anything for any length of time. I couldn’t read a book without falling asleep, and ditto with trying to watch anything on the television. I could, however, do jigsaw puzzles. Friends supplied me with some tricky ones… and I enjoyed sitting at the table and doing them.

“Life is very boring,” I wrote in my diary. “There seems little to look forward to, and the worst is yet to come. But I’m still here!”
It was hard not to mull over the things I hadn’t done, wasn’t currently doing, and wasn’t going to do. For instance, I had cancelled my holiday in Kenya and was involved in the protracted procedure of claiming on my travel insurance. I was supposed to meeting up with a group of old NHS friends for an annual get together and dinner, but had to cancel that. Meanwhile, a dear group of University friends were going away for our annual Christmas celebration – a week in a country house – and I couldn’t join them. Our pre-Christmas traditions of seeing the lights at Dunham Massey, and going to the Christmas Eve music concert at the Bridgewater Hall would have to happen without me. And I had a holiday booked in the Maldives for January. That had to be cancelled to.
How did I cope with it all? I spent much of my time asleep and, fortunately, I slept very well. I also tried to focus only on the next few days – to look forward to a friend coming to visit, a phone call, or one of my daughters popping in. Or starting the next jigsaw puzzle.
I was still eating. Soft food. I had even learnt how to poach an egg… I was quite pleased with this one.

All that changed after my third chemo-infusion, which I had on the 22nd November.
The best thing about this infusion was they had trouble booking me in, because my chemo had been rearranged from last week and all the chairs in the unit were fully booked for this day. So, all they could offer me was a bed. A bed! Perfect. I slept the whole day through, only getting up once to make the 2 yards trip to my very-own ensuite toilet!
The dose of chemo was lowered a little (I had mixed feeling about that – pleased the side effects might be less, but worried I was giving the cancer a free ride). But, even with the lower dose, I still felt terrible afterwards when the steroids wore off. In fact, I felt terrible all the time.
I was having to rest after the most minor exertion. After climbing stairs, I would need to sit down for 20 minutes for a rest. Housebound now, the only outings I had were for my radiotherapy sessions. Friends and family came round and changed my sheets, made my bed, put on the washing, took out the washing, and generally looked after me.
“It’s so frustrating,” I wrote in my diary. “These might be the last few weeks or months of my life, and I am just marking time.”
On the first Sunday in December, my swallowing became a major problem. I had difficulty getting even a yoghurt down, and and realised I was avoiding drinking anything – even avoiding water. I couldn’t get my chemotherapy tablets down, and they were tiny. So I had to start using my RIG – the tube that had been punched through my abdomen and into my stomach.
This meant, I had to draw up this horrible sickly stuff in a giant syringe and slowly push it through the tube and into my stomach. I then had to flush the RIG tube through with boiled water. And then I had to wash the syringe out carefully. The whole thing seemed such an effort. And, even though I wasn’t actually tasting the sickly fluid, it still made me feel sick when it entered my stomach.
I cried on the Monday. The first real tears I had shed.
On the Tuesday, I saw the doctor in the radiotherapy department for a routine review. She said I looked very well, and most patients were much worse than me at this stage. Dread to think what the other patients must have looked like!
I was having trouble getting enough calories down the JIG tube too, because just preparing the feeds took such an effort. My twice-daily chemo tablets had to be crushed up, dissolved in warm water (not boiling) and fed down the JIG tube too. Then everything had to be washed up. It was a huge effort to do all this.
“Life is barely worth living,” I wrote in my diary. “I want my old life back.”
My last IV session was on Wednesday, the 13th December, and my daughter, Annie, offered to come and stay the night. On the Monday, she came round with a Christmas tree and put it up for me and decorated it. At least the house looked Christmassy, but I certainly didn’t feel it.
The nurses offered me a bed for the last session. I was delighted. Another day of sleeping. When they woke me up to tell me I could go home, everybody else had left.
Now, it is a tradition to RING THE BELL after your last chemo session. I hadn’t been planning on doing this, after all, I still had another few days of radiotherapy to go and the end of therapy didn’t mean the end of cancer. But the nurses seemed very keen and, in the absence of any other patients to applaud, they left their various posts and came to stand in the corridor to watch.
So, I rang the bell, and the nurses applauded. And they took a photo. And here it is…

Look at my hair! If I look as though I’ve just been dragged out of bed, well, that is exactly what has just happened!
Two days later on the Friday, I had my 25th, and final, radiotherapy session. I was so weak, my daughter Annie had to wheel me into the department (the Christie has a supply of wheelchairs to borrow at the entrance to the hospital). I looked around at all the other patients in wheelchairs and remembered how I bounced in on my first day, glad I wasn’t as ill as the rest of the patients. Now, I was in a wheelchair too!
The technician who looked after me for the last seesion was a young lady I had met several times before. “Well done,” she said. And gave me a hug.
Afterwards, I RANG THE BELL in the radiotherapy department, and my daughter filmed it.
The next week, on Wednesday the 20th December, I wrote this in my diary:
Tomorrow is the shortest day. After that, things WILL get better. Days will get longer. I will feel stronger. My swallowing will improve. Can’t wait to get back to walking. Can’t wait to start eating again. I am currently craving gravy and roast potatoes. All the Xmas food adverts on TV are killing me.
I did feel happy to have rung the bell (twice) but I wouldn’t find out if the treatment had worked or not for another 3 months, when I was due a follow-up scan. I planned to make the most of the three months before the scan, to take every day as it comes, and to enjoy what I could before I found out if the treatment had worked or not.
Actually, I was feeling cautiously optimistic. I had done everything I could do to defeat the cancer and I couldn’t have done anything more. I started from a position of strength and, despite my tiredness and swallowing problems, my body still seemed healthy. I had kept my hair. My finger nails were still growing. My skin was in good condition. I had no neurological side-effects (apart from some mild tinnitus) and my mind was still sharp. I didn’t feel like a terminally-ill patient.
I wrote in my diary, “I’m bored. This is a good sign.” And I set off to finish my latest jigsaw.
Actually, things did get worse before they got better. I had been warned that after radiotherapy I would continue to deteriorate for another two weeks. But, the next day, I could barely get out of bed and felt so dizzy when I stood up that I was having to hold onto the walls in order to walk. I had a phone conversation with the specialist nurse, and she arranged for me to be admitted to the assessment unit at the Christie the following day. Eldest daughter took the day off work to take me in.
Turns out that I hadn’t been giving myself enough fluids through the RIG tube, and had ended up dehydrated with very low blood pressure. The doctors at the Christie gave me a bag of intravenous fluid, and I perked up.
My eldest daughter stayed with me over Christmas, only leaving to join her husband’s family for a Xmas meal. I can honestly say it was the worst Xmas I had ever had. The only food I ate was sickly Ensure fluid, fed in through the RIG tube. I still felt exhausted when I tried to do anything and relied on other people to change my sheets, sort my washing out, etc.
But, slowly, I began to improve. On New Year’s Eve (the first New Year’s Eve I have spent on my own) I stayed up to watch the firework display. And then, on the 2nd of January, 2024, I ate my first food for weeks – a scrambled egg.
[To be continued…]






A very difficult journey for you Ruth, I’m glad you had the support of your family and friends. My ex partner’s brother is currently going through cancer treatment – something to do with the lymph nodes – and he’s been going through much of what you describe here, plus he’s had a recurring C-diff infection and three hospital admissions because of it. I’m keeping my fingers crossed that he comes through it, and the fact that you are now writing this shows you are on the up side – all the best, and please update us when you can xx
It is testament to the tough regimen of treatment. You have a particular and rare strength, yet it sounds like there were really tough moments. It may have flexed you, but you did not break. Well done.
Best wishes and God speed … You will beat this. After all, you have to finish your grand endeavour…
How awful for you. I’m glad you got to see a puffin first – very cheering birds.
We walkers just keep on plodding along, through everything.
What a lovely jigsaw, I have just spotted the owl shaped piece in the middle. I had spotted the bell ringing photo on Facebook, what a lot you have been through. Hopefully now it is onwards and upwards. Chocolate can be very helpful, just remember fruit and nut will contribute to your 5 a day.
🫂
Hi Ruth – I have everything X’d that you are now through the worst of this (insert bad word 🙂 ) sickness.
As ever my very best wishes – Cheers Russ
We have exchanged emails, thanks.
How do you poach your eggs?
I hope the last piece of the jigsaw fit.
I much like that beach photo with the figures – very atmospheric.
In France when you meet fellow randonneurs , as we go on our respective ways they say “Bonne continuation.”
I haven’t got an egg poacher, because you SHOULD be able to poach an egg without one. With this attempt, I cracked the egg into a ladle and lowered it slowly into boiling water. I’ve tried various other techniques with little success!
I found out recently (from Masterchef or something similar) that you should have the water on a rolling boil, and it does seem to help. My efforts are always blighted by the fact that even after 50-odd years of practice I still can’t adequately crack an eggshell without ending up with eggs full of shell, or a broken yolk! I often say that if I could elect to have a superpower I would choose that….
so sad, we wish you well and improved health. We enjoy going to Dunham Massey and also Arley Hall and Gardens. the cafe at Arley is very good
What has happened to you just about completely mimics my situation so I feel very much for you. My last coastal walk was in February 2023 after which I was diagnosed with bowel cancer. Went through all the chemo and radiotherapy and had the operation May. I didn’t have the RIG tube that sounds terrible But I had some time with a tube in my nose down to the stomach. I am still trying to recover my strength and getting back to the coastal walk is a major objective.
You have my best wishes for your recovery.
Keith
I’m so sorry to hear this, Keith. It takes a long time to recover, doesn’t it. Wishing you all the best.
What a difficult time you have been through. My best wishes, as ever.
my god you are one brave lady ,love and prayers
That’s brutal, absolutely brutal no other way to describe it. I am so sorry to hear what you had to go through. I mean I didn’t expect cancer treatment to be good but I didn’t realise quite how awful it is. I hope you are able to pull through (I guess the fact you are still writing this is a good sign!). I am really not sure I could have handled it. Perhaps your fitness from all your walking helped here?
I hope you are able to get back to doing things you enjoy. I also appreciate you sharing this (I know it’s quite personal) as I find it an eye opener as to what it’s like and I am sorry you had to experience it.
I was so shocked and sad to read about your diagnosis. I have done a lot of coast walks (random) and always read your blogs before I do a section.
My husband was diagnosed with adenocarcinoma of his oesophagus in 2007 and had a big operation (Ivor Lewis). A large number of lymph nodes were infected, the cancer was diagnosed far too late.
Your fitness from all your walking and your brave attitude will get you through this.
So sorry to hear about your husband. It’s a horrible disease.
Dear Ruth,
What a dreadful shock for you and your family. We were so sorry to hear your news. Clive and I wish you all very very best for your recovery. You are one very brave lady. With our best wishes Vivien and Clive (Stamford)
Hi Ruth,
I am echoing the above wonderful sentiments from your dedicated and caring blog readers/friends. Thanks for sharing your recent story with all of it’s difficulties and also, sharing the support of your family and friends. Warmest wishes
Robin
I’m so sorry to hear this and wish you all the best. I’ve been following your progress over the years (mostly in lurking mode) and have enjoyed getting to ‘know’ you through your comments and style of writing. It’s a shock to hear about your diagnosis and treatment, especially as my partner is currently having treatment for (incurable) lung cancer, having been diagnosed around the same time last year. I recognise a lot of the things you are going through and understand how even the simplest things can grind you down, or take forever to complete. We often wonder how people cope with cancer treatment when they or their partners have to go to work to pay the bills, it really is a ‘full time job’!
So sorry to hear about your husband, Helena. I’ve no idea how some people manage to work during treatment. Some people in the chemo unit were obviously working – came in work suits, used their laptops, had their 30mins of chemo and left. I could barely manage a jigsaw puzzle!
Wishing you all the best. During this horrible time. The only thing worse than enduring it yourself is watching someone you love.